Telemedicine911™
Emergencies Happen.
The Missing Link for a Complete Telemedicine Program
Already have an account? Sign in here.
Understand the Problem
911 Recordings
Listen to real 911 recordings from video visits, RPM, voicemail, and telephone encounters and learn about common emergencies
9-1-1 Barriers
Learn about United States 911 infrastructure problems and use tips
Regulation and Law
Current Rules and Regulations that impact patient care during a Telehealth emergency.
Patient Behavior
Do patients follow through on what we ask them to do?
Risk and Return
Review the odds of failure, lawsuits, and financial losses / returns.
Successes
Learn about best practices, clinical guidelines, and clinical cases.
Faulty Protocols
Learn about the failures of other telemedicine programs.


What are some common emergencies during telemedicine?
Common Emergencies During Telemedicine
- Video Visit: A patient is on a standard video conference with her doctor and says she wants to commit suicide and explains how she wants to do it. She is cutting herself on the video.
- Video Visit: A patient has an expedited appointment and is COVID+, tachypneic, tachycardic, and “looks sick” on video.
- Remote Patient Monitoring Video Visit: A compliant patient was not feeling well and took her vitals and a finger stick. Glucose was “high” on Glucometer (over 600).
- Voicemail: A patient with a known history of depression leaves a voicemail with her healthcare practice. She said on voicemail, “I want to kill my neighbor and drive off a cliff.”
- MCT (Mobile Cardiac Telemetry): The monitoring device alerted for SVT but the patient was normotensive.
What is your emergency protocol now?
Below are a list of current protocols and the challenges associated:
-
Call 911 on behalf of patient
- Reaching the incorrect 911 dispatch center
- Incorrect location sent to 911
-
Instruct patient to call 911 or go to ER
- Patient does not comply
-
Maintain a list of dispatch and ambulance contacts
- Out of date lists
- Priority Two numbers have longer hold times
-
Escalation to other managers, staff, and nurses
- Time and resources used

How It Works
By easily integrating into your existing telemedicine platform, your staff can provide a reliable and compliant handoff at a level of service your patient deserves.
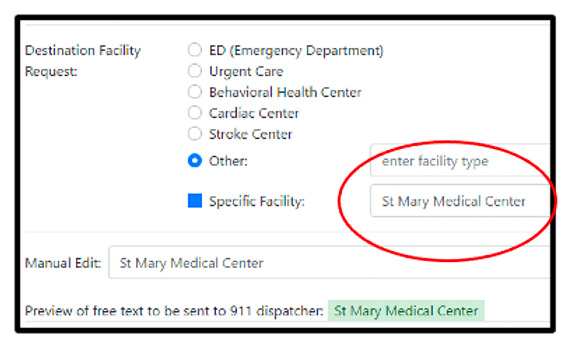
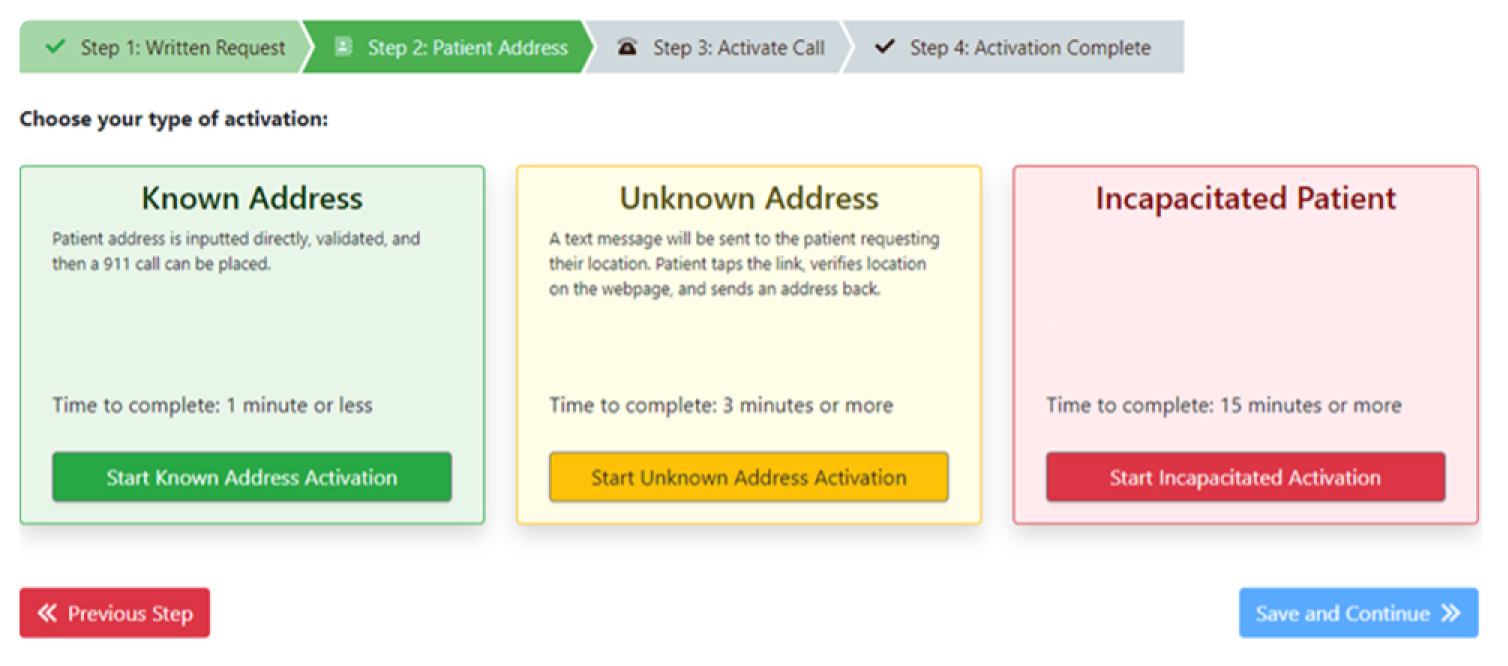
Step 1 Enter Text Request
Enter your patient’s name, request ALS or BLS response, and request the destination facility. When you talk to 911, this text will be sent to the 911 dispatcher handling the case.
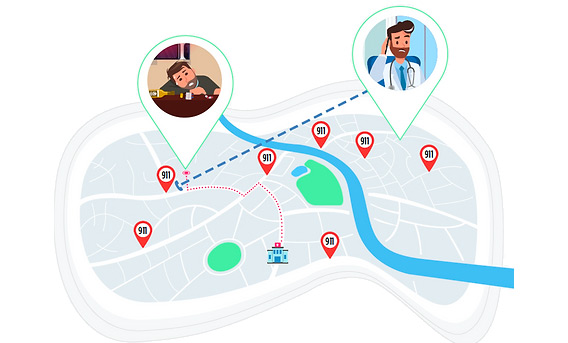
Step 2 Air®GeoLocate
Use GPS locate the patient’s mobile device or enter the patient’s location to ensure the ambulance goes to the correct address, room, and floor.
Step 3 Talk to 911
Talk directly to the 911 dispatcher where your patient Is located. On-screen guidance helps reduce medical error and improve outcomes.
Handle Different Scenerios
911 jurisdiction routing by latitude & longitude
When your patient is on the road, our geolocation tool, Air®GeoLocate, will pull the real time latitude and longitude of the patient’s location, route your communication to the correct 911 jurisdiction servicing your patient’s zone, and document the latitude and longitude for the 911 dispatcher handling your case. There are no apps to download. We keep it simple, calm, and reliable for your staff, 911 dispatchers, and your patients.

Maintaining Level of Care
Quality handoff has proven to help
The Joint Commission recommends all hand-off procedures to have both written and verbal components. These types of handoff requirements have been shown to reduce medical error and adverse events.
New England Journal Of Medicine; 2014; 371(19) Starmer
Improve your transition of care from
telehealth to 911 dispatchers
Enroll Today!
Schedule a Demo
Need more info? Contact us today!